Estrogen and progesterone are two major female sex hormones.
In addition to the regulation of reproductive function, estrogen is also a master regulator of many critical body functions, while progesterone may exert synergistic and antagonistic (or opposing) function to estrogen.
The balance of these two hormones play vital roles to many aspects of women’s health, not just reproductive health.
There are two main manifestations of imbalance between estrogen and progesterone:
- Estrogen excess or dominance (i.e., high estrogen-to-progesterone ratio) and
- Estrogen deficiency.
Each of these manifestations can contribute to many pathologies and functional disorders in the body.
Estrogen excess/dominance is more prominent among premenopausal (including perimenopausal) women and is associated with uterine fibroid, endometriosis, breast cancer, endometrial cancer, premenstrual syndrome (PMS) and perimenopausal symptoms1–6.
Estrogen deficiency occurs primarily during postmenopausal period, and is associated with subjective menopausal symptoms, and chronic degenerative diseases including osteoporosis, cardiovascular diseases (CVDs) and cognitive decline7–9.
Hormonal imbalance is often not the root of the problem, but rather an outcome of other underlying dysfunctions and stressors in the body (see Why Stress is the Culprit).
Learn more about how Functional Health Coaching can help you uncover and address the hidden stressors contributing to your hormonal imbalance.
Estrogen and Progesterone: The Balancing Act
Estrogen and progesterone may act synergistically or antagonistically with one another depending on the target organs and body functions (see Figure 1).
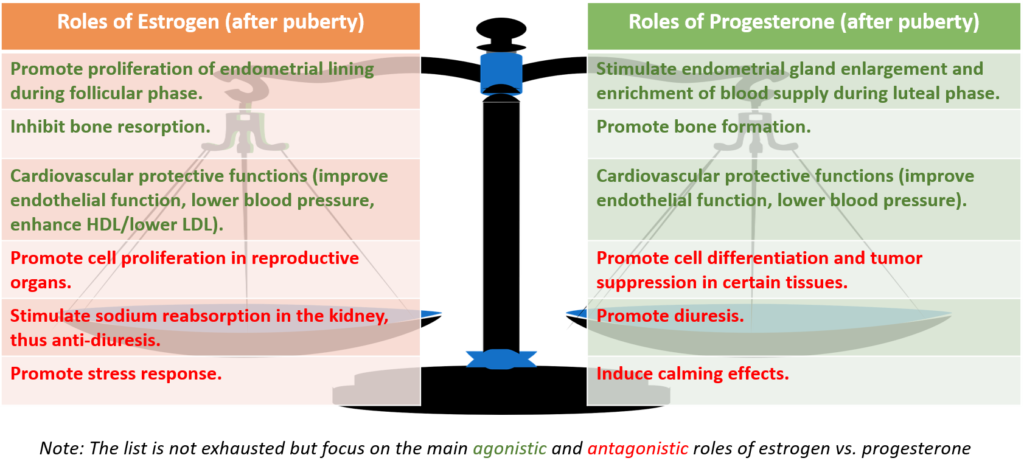 Figure 1. Estrogen and Progesterone: The Balancing Act
Figure 1. Estrogen and Progesterone: The Balancing Act
Estrogen and progesterone work concertedly to establish and regulate menstrual cycles. Estrogen promotes proliferation of endometrial lining of the uterus during the first half of a menstrual cycle, while progesterone stimulates enlargement of endometrial gland and enrichment of blood supply to endometrial tissues during the second half of a menstrual cycle.
Both estrogen and progesterone promote bone health, wherein estrogen inhibits bone resorption and progesterone promotes bone formation.
Both hormones have protective effects on heart/cardiovascular health including lowering blood pressure and improving HDL-to-LDL ratio1,10,11.
Several antagonistic roles of estrogen and progesterone are shown in Figure 1:
- Estrogen promotes cell proliferation in reproductive organs including the breast and the uterus, hence when in excess can lead to tumor growth.
- Progesterone promotes cell differentiation and tumor suppression in particular in endometrial tissues of the uterus and in some cases in breast cancer cells. Note that progesterone exerts agonistic effect with estrogen in promoting the growth of uterine fibroids.2,4,5
Estrogen Excess/Dominance: Causes, Associated Pathologies, and Symptoms
Causes
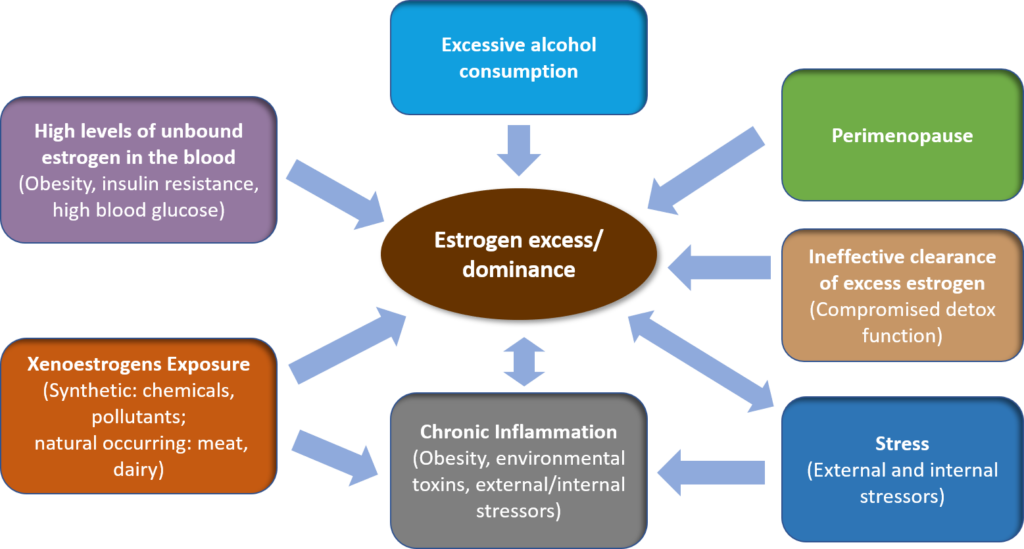
Several contributing factors to estrogen excess or dominance have been identified in clinical and preclinical studies (see Figure 2).
These factors include xenoestrogen exposure, perimenopause, chronic inflammation, high levels of unbound/bioavailable estrogen in the blood, ineffective clearance of excess estrogen in the body, stress, and excessive alcohol consumption.
Figure 2. Contributing Factors to Estrogen Excess/Dominance
Xenoestrogen Exposure
Xenoestrogens are externally present or foreign compounds that exert estrogenic effects in the body. Xenoestrogens can be synthetic or natural occurring substances.
Synthetic xenoestrogens
These are widely used industrial chemicals including parabens, phthalates, nitro musks, benzophenones, polychlorinated biphenyls (PCBs), polybrominated biphenyls (PBBs), bisphenol A (BPA), pesticides, fungicides and fire retardants that are often found in environmental pollutants, food additives, personal care and cosmetic products, and household consumables.
Fish consumption can increase exposure to persistent organic pollutants (POPs) including PCBs, PBBs and pesticides, which has been associated with increased incidents of uterine fibroids and endometriosis.
Estrogen-containing oral contraceptives and hormone replacement therapy (HRT) are also synthetic xenoestrogens that can contribute to estrogen excess/dominance 2,11,12.
Naturally occurring xenoestrogens
These are found in plant foods, i.e., phytoestrogens, and endogenous estrogen in animal tissues.
Certain phytoestrogens such as soy and flaxseed exert regulating effects to the endogenous estrogen in the body. These phytoestrogens can counter-balance estrogen excess/dominance as well as estrogen deficiency, hence reducing the risks of estrogen excess/dominance related disorders (including breast cancer, endometrial cancer and ovarian cancer) and postmenopausal estrogen deficiency related disorders (including menopausal symptoms, CVDs, osteoporosis and cognitive decline)13–20.
Naturally occurring estrogen is also found animal meat products and dairy products.
Meat and dairy consumption have been found to raise the estrogen levels in blood and urine21. Population studies have shown the correlation between dairy product intake and increased risk of some estrogen excess/dominance related cancers (including breast cancer, ovarian cancer, uterine cancer and endometrial cancer)22–24.
Perimenopause
Perimenopause is a period of about 6 to 9 years before menopause during which a woman experiences erratic fluctuation and relative increase in estrogen levels, and relative reduction progesterone levels.
During perimenopause, the hormone feedback loop between the brain (i.e., the hypothalamus and the pituitary gland) and the ovaries is disrupted. Anovulation may occur, resulting in irregular menstrual cycles and bleeding1,9.
Chronic Inflammation
Chronic inflammation caused by obesity, environment toxins, and external and internal stressors can stimulate the synthesis of estrogen in the body, resulting in estrogen excess/dominance and associated pathologies25,26.
Estrogen can in turn potential inflammatory response in the body, thus forming a vicious “feed forward” cycle27,28.
High Levels of Unbound/Bioavailable Estrogen in the Blood
Estrogen is transported in the blood by a protein called the sex hormone binding globulin (SHBG).
When estrogen is bound to SHBG, it does not exert estrogenic effects in the body. Therefore, the lower the SHBG levels, the higher the risk of estrogen excess/dominance.
Obesity, insulin resistance, high blood sugar levels have been found to correlate with reduced SHBG levels, and increased risk of estrogen excess/dominance and estrogen-dependent cancers (including breast cancer, ovarian cancer and endometrial cancer)29,30.
Ineffective Clearance of Excess Estrogen in the Body
The liver is the primary detoxification organ in the body. Under normal condition, the liver metabolizes excess estrogen into inactive compounds, which are then secreted with bile into the small intestine and excreted through bowel movements.
However, any dysfunction in the liver detoxification process, bile synthesis and secretion by the liver/gallbladder, and elimination function of the large intestine/colon can result in increased estrogen levels in the body and increased risk of diseases associated with estrogen excess/dominance27,33,34.
Chronic Stress
Chronic stress elevates cortisol levels and can deplete progesterone levels because cortisol is synthesized from progesterone in the adrenal glands. Reduced progesterone levels with respect to estrogen levels contribute to estrogen dominance.
In addition, estrogen can potentiate the stress response in the body and elevate cortisol levels.
Therefore, stress and estrogen excess/dominance can form a vicious cycle1,3. (Learn more about Why Stress is the Culprit)
Excessive Alcohol Consumption
Alcohol consumption of more than 15 g/day, or five or more glasses of wine per week was shown to increase estrogen levels in the blood by more than 20%31,32.
Associated Pathologies and Symptoms
Clinical studies have shown the association between estrogen excess/dominance and the following pathologies and overt symptoms:
- Increased risk of certain forms of cancers including breast cancer, endometrial cancer, endometriosis, uterine fibroid, polycystic ovarian syndrome (PCOS), ovarian cancer and prostate cancer4,11.
- Increased risk of autoimmune diseases11.
- Subclinical or clinical hypothyroidism (potentiated by chronic stress and estrogen excess/dominance)6.
- Perimenopausal symptoms including mood swings, dry mouth, tachycardia (rapid heart rate), chest pain, weight gain, fluid retention, mastalgia (breast pain)1.
- Increased PMS including anxiety, insomnia, irritability, irregular bleeding, spotting prior to start of menstruation, fluid retention, weight gain, headaches or migraines, mastalgia, and menstrual pain and cramps3.
Estrogen Deficiency: Causes, Associated Pathologies and Symptoms
Causes
The major contributing factors to estrogen deficiency are menopause and suppressed estrogen synthesis (see Figure 3).
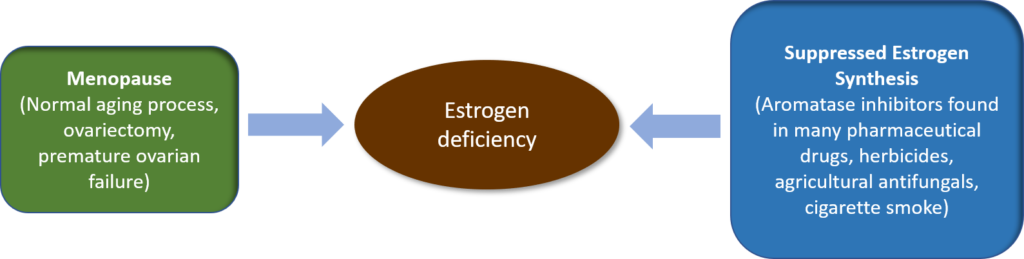 Figure 3. Contributing Factors to Estrogen Deficiency
Figure 3. Contributing Factors to Estrogen Deficiency
Menopause
Menopause can be a normal aging process or can be caused by ovariectomy and premature ovarian failure. Premature ovarian failure may be idiopathic or associated with autoimmune disorders, chromosomal abnormality or toxic exposure.
During menopause and postmenopause, ovarian production of estrogen and progesterone, and menstrual cycle cease.
The ovaries and the adrenal glands continue to produce androgens. Other body sites, primarily fat tissues, and other sites including breasts, skin, brain, bone and liver continue to produce small amounts of estrogen through synthesis of estrogen from androgens7,11.
Suppressed Estrogen Synthesis
Another important contributor to estrogen deficiency is the use or exposure to chemicals that inhibit the enzyme (called aromatase) responsible for the synthesis of estrogen from androgens (see Figure 3).
Aromatase inhibitors are found in:11:
- Many pharmaceutical drugs, including antidepressants, antipsychotics, anticonvulsants opiates, anti-androgens, anti-hypertensive drugs, H2-receptor antagonists, antimalarials, anticancer drugs, and immunosuppressive drugs comprising glucocorticosteroids and methotrexate
- Herbicides such as glyphosates and Roundup
- Azole compounds in agricultural antifungals
- Cigarette smoke
Associated Pathologies and Symptoms
Apart from its roles in reproductive organs and reproduction, estrogen is also a master regulator of many critical body functions, including glucose metabolism, lipid homeostasis and regulation of body fat distribution, immune function, brain and nervous system function, bone mineralization, and epiphyseal closure.
Estrogen also exerts protective effects on the cardiovascular system by protecting against arteriosclerotic vascular disease.
The many subjective symptoms and chronic degenerative diseases associated with postmenopause are associated with rapid decline of estrogen levels11.
Clinical studies have shown the association between estrogen deficiency and the following pathologies and overt symptoms7–9:
- Menopausal symptoms that occur during late perimenopause (i.e., 1-3 years prior to menopause) and early postmenopause (i.e., first 2 years of postmenopause) including hot flushes, mood swing, nervousness, heart palpitation, sleep disturbance, fatigue, weakness, joint and muscle pain, headache, and difficulty concentrating.
- Chronic degenerative diseases including obesity, abnormal blood lipid levels, CVDs, osteoporosis, joint pain, insulin resistance and diabetes, urogenital atrophy, cognitive decline, Alzheimer’s disease, Parkinson’s disease, and increased risk of kidney diseases among diabetics.
- Increased risk of eclampsia and pre-eclampsia during pregnancy.
Nutrition and Lifestyle Approaches for Female Hormonal Health
Holistic approaches encompassing nutrition and lifestyle can be used to address the modifiable contributing factors to estrogen excess/dominance and estrogen deficiency.
In addition, nutrition and lifestyle approaches can also help to regulate estrogen and progesterone levels and actions in the body.
Learn more about Diet and Nutrition for Female Hormonal Health, and Lifestyle Approaches for Female Hormonal Health.
Related Articles
Diet and Nutrition for Female Hormonal Health
Lifestyle Approaches for Female Hormonal Health
References
- Prior J. The endocrinology of perimenopause need for a paradigm shift. Frontiers in Bioscience. 2011;S3(2):474-486. doi:10.2741/s166
- Trabert B, Chen Z, Kannan K et al. Persistent organic pollutants (POPs) and fibroids: results from the ENDO study. J Expo Sci Environ Epidemiol. 2014;25(3):278-285. doi:10.1038/jes.2014.31
- Bunzenmeyer J. Pre-Menstrual Syndrome: The Orchestration of Hormones. Ndnr.com. http://ndnr.com/womens-health/pre-menstrual-syndrome-the-orchestration-of-hormones/. Published 2018.
- Kim J, Kurita T, Bulun S. Progesterone Action in Endometrial Cancer, Endometriosis, Uterine Fibroids, and Breast Cancer. Endocr Rev. 2013;34(1):130-162. doi:10.1210/er.2012-1043
- Edwards L, Heyman A, Swidan S. Hypocortisolism: An evidence-based review. Integrative Medicine A Clinician’s Journal. 2011;10(4): 30-37.
- Tahboub R, Arafah B. Sex steroids and the thyroid. Best Practice & Research Clinical Endocrinology & Metabolism. 2009;23(6):769-780. doi:10.1016/j.beem.2009.06.005
- Dalal P, Agarwal M. Postmenopausal syndrome. Indian Journal Of Psychiatry. 2015;57(6):222. http://dx.doi.org/10.4103/0019-5545.161483
- Bergamini C, Cervellati C. Oxidative damage and the pathogenesis of menopause related disturbances and diseases. Clinical Chemistry And Laboratory Medicine (CCLM). 2016;54(5):739-753. http://dx.doi.org/10.1515/cclm-2015-0807
- Hale G, Robertson D, Burger H. The perimenopausal woman: Endocrinology and management. J Steroid Biochem Mol Biol. 2014;142:121-131. doi:10.1016/j.jsbmb.2013.08.015
- Marieb E, Hoehn K. Human Anatomy & Physiology (10th ed). San Francisco, CA: Pearson Benjamin Cummings; 2016
- Patel S, Homaei A, Raju A, Meher B. Estrogen: The necessary evil for human health, and ways to tame it. Biomedicine & Pharmacotherapy. 2018;102:403-411. doi:10.1016/j.biopha.2018.03.078
- Fucic A, Gamulin M, Ferencic Z et al. Environmental exposure to xenoestrogens and oestrogen related cancers: reproductive system, breast, lung, kidney, pancreas, and brain. Environmental Health. 2012;11(Suppl 1):S8. doi:10.1186/1476-069x-11-s1-s8
- Gencel V, Benjamin M, Bahou S, Khalil R. Vascular Effects of Phytoestrogens and Alternative Menopausal Hormone Therapy in Cardiovascular Disease. Mini-Reviews In Medicinal Chemistry. 2012;12(2):149-174. http://dx.doi.org/10.2174/138955712798995020
- Wei P, Liu M, Chen Y, Chen D. Systematic review of soy isoflavone supplements on osteoporosis in women. Asian Pac J Trop Med. 2012;5(3):243-248. doi:10.1016/s1995-7645(12)60033-9
- Thaung Zaw J, Howe P, Wong R. Does phytoestrogen supplementation improve cognition in humans? A systematic review. Ann N Y Acad Sci. 2017;1403(1):150-163. doi:10.1111/nyas.13459
- Chen M, Lin C, Liu C. Efficacy of phytoestrogens for menopausal symptoms: a meta-analysis and systematic review. Climacteric. 2015;18(2):260–269. http://doi.org/10.3109/13697137.2014.966241
- Fritz H, Seely D, Flower G et al. Soy, Red Clover, and Isoflavones and Breast Cancer: A Systematic Review. PLoS ONE. 2013;8(11):e81968. doi:10.1371/journal.pone.0081968
- Myung S, Ju W, Choi H, Kim S. Soy intake and risk of endocrine-related gynaecological cancer: a meta-analysis. BJOG: An International Journal of Obstetrics & Gynaecology. 2009;116(13):1697-1705. doi:10.1111/j.1471-0528.2009.02322.x
- Zhang G, Chen J, Liu Q, Zhang Y, Zeng H, Zhao Y. Soy Intake Is Associated With Lower Endometrial Cancer Risk: A Systematic Review and Meta-Analysis of Observational Studies. Medicine (Baltimore). 2015;94(50):e2281. doi:10.1097/md.0000000000002281
- Calado A, Neves P, Santos T, Ravasco P. The Effect of Flaxseed in Breast Cancer: A Literature Review. Front Nutr. 2018;5. doi:10.3389/fnut.2018.00004
- Harmon B, Morimoto Y, Beckford F et al. Oestrogen levels in serum and urine of premenopausal women eating low and high amounts of meat. Public Health Nutr. 2013;17(09):2087-2093. doi:10.1017/s1368980013002553
- Ludwig D, Willett W. Three Daily Servings of Reduced-Fat Milk. JAMA Pediatr. 2013;167(9):788. doi:10.1001/jamapediatrics.2013.2408
- Regal P, Cepeda A, Fente C. Development of an LC-MS/MS method to quantify sex hormones in bovine milk and influence of pregnancy in their levels. Food Additives & Contaminants: Part A. 2012;29(5):770-779. doi:10.1080/19440049.2011.653989
- Lu W, Chen H, Niu Y, Wu H, Xia D, Wu Y. Dairy products intake and cancer mortality risk: a meta-analysis of 11 population-based cohort studies. Nutr J. 2016;15(1). doi:10.1186/s12937-016-0210-9
- Patel S. Disruption of aromatase homeostasis as the cause of a multiplicity of ailments: A comprehensive review. J Steroid Biochem Mol Biol. 2017;168:19-25. doi:10.1016/j.jsbmb.2017.01.009
- Zahid H, Simpson E, Brown K. Inflammation, dysregulated metabolism and aromatase in obesity and breast cancer. Curr Opin Pharmacol. 2016;31:90-96. doi:10.1016/j.coph.2016.11.003
- Evans J. An Integrative Approach to Fibroids, Endometriosis, and Breast Cancer Prevention. Integrative Medicine. 2008;7(5):28-31.
- Monteiro R, Teixeira D, Calhau C. Estrogen Signaling in Metabolic Inflammation. Mediators Inflamm. 2014;2014:1-20. doi:10.1155/2014/615917
- Daka B, Rosen T, Jansson P, Rastam L, Larsson C, Lindblad U. Inverse association between serum insulin and sex hormone-binding globulin in a population survey in Sweden. Endocr Connect. 2012;2(1):18-22. doi:10.1530/ec-12-0057
- Goldštajn M, Toljan K, Grgić F, Jurković I, Baldani D. Sex Hormone Binding Globulin (SHBG) as a Marker of Clinical Disorders. Coll Antropol. 2016;40(3):211-218.
- Hartman T, Sisti J, Hankinson S et al. Alcohol Consumption and Urinary Estrogens and Estrogen Metabolites in Premenopausal Women. Hormones and Cancer. 2016;7(1):65-74. doi:10.1007/s12672-015-0249-7
- Playdon M, Coburn S, Moore S et al. Alcohol and oestrogen metabolites in postmenopausal women in the Women’s Health Initiative Observational Study. Br J Cancer. 2017;118(3):448-457. doi:10.1038/bjc.2017.419
- Hodges R, Minich D. Modulation of Metabolic Detoxification Pathways Using Foods and Food-Derived Components: A Scientific Review with Clinical Application. J Nutr Metab. 2015;2015:1-23. doi:10.1155/2015/760689
- Goldin B, Adlercreutz H, Gorbach S et al. Estrogen Excretion Patterns and Plasma Levels in Vegetarian and Omnivorous Women. New England Journal of Medicine. 1982;307(25):1542-1547. doi:10.1056/nejm198212163072502