Join our mailing list to receive the latest health tips and updates.
You have Successfully Subscribed!
How Toxins Affect Your Health and Tips to Reduce Toxic Load
The word ‘Detox’ may become increasingly common and even trendy these days. You may have heard of people telling you that they are going through some detox or cleansing protocol.
So, what is detox, and do we need it?
In our modern living, toxins are ubiquitously present in our daily life, in our foods, environment, personal care and household products, etc. We may be exposed to as many as tens of thousands of toxins on a regular basis.
Do you have some lingering health conditions or simply not feeling your best, e.g. chronic fatigues, joint pain and other aches and pains, digestive issues, sleep issues, skin issues, lack of mental clarify and brain fog, mood swing, etc?
You may try to eat healthy, do regular exercise, try various health modalities, but still could not shake off these lingering health issues.
Have you considered toxins as one of the potential culprits to your health challenges?
Numerous scientific studies have shown that toxin exposure is associated with widespread adverse health effects that are so prevalent in our modern society, including hormonal disruption, reproductive dysfunction, digestive/gut disorders, allergies and sensitivities, metabolic disorders/diseases (incl. obesity, type 2 diabetes, heart disease, hypertension, etc.), brain, neurological and mental disorders, cancer, immune dysfunction and autoimmune disorders, chronic liver disease, chronic kidney disease, etc.
In this article, I share evidence-based information on common toxins we encounter in everyday life, how toxins affect our health and tips to reduce toxic load in your body.
For a quick summary of the tips to reduce toxic load in your body, you can go directly to the Summary section.
For a summary video presentation, please check out my YouTube video below:
Topic List
Common Toxins We are Exposed to
The Body’s Natural Detoxification Capabilities
Endocrine (or Hormone) Disruption
Brain, Neurological and Mental Disorders
Damage to Detox Organs (Liver, Kidneys, Gut)
Impaired Lung and Respiratory Health
Tips to Reduce Toxic Load in the Body
Support Detox Organs and Drainage Channels
Employ Specific Detox Protocol
Summary
Toxins can come from external sources or generated internally in our body. Common toxins we are exposed to are summarized in section Common Toxins We are Expose to.
Our body has strong natural detoxification capability, as summarized in section The Body’s Natural Detoxification Capabilities.
However, when we are bombarded with tens of thousands of toxins in modern living, the natural detox capabilities of our body can be overwhelmed, resulting in many adverse health effects, as described in section How Toxins Affect Our Health?
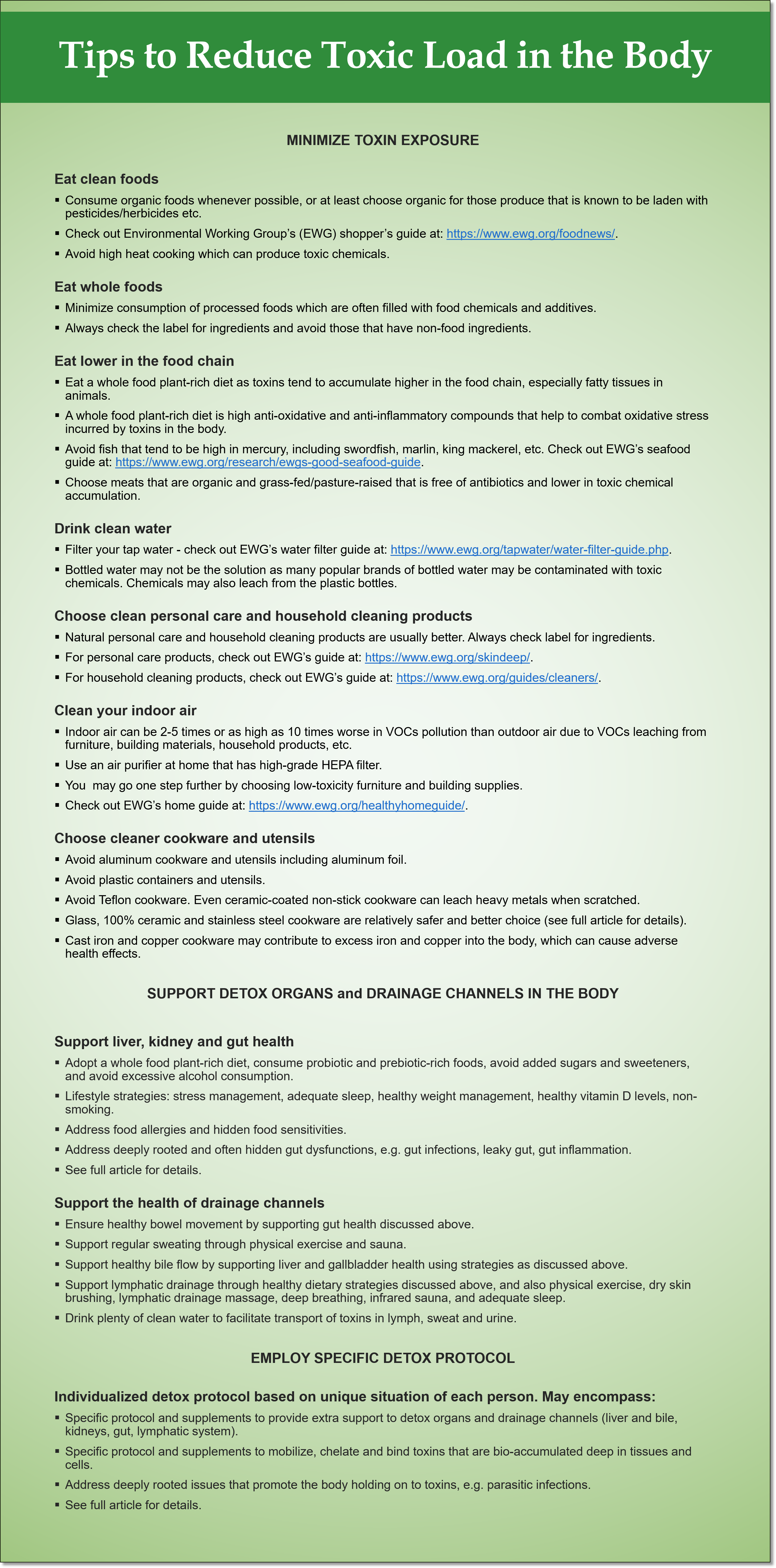
A summary of tips to reduce toxic load in the body is given below (for more details, see section Tips to Reduce Toxic Load in the Body).
Common Toxins We are Exposed to
What are toxins? Toxins are unwanted substances in the body that cause adverse biological reactions.
Toxins can be from external sources that we are exposed to or generated internally in our body.
External Sources of Toxins

Figure 1. Various sources of man-made toxins
External sources of toxins are also called xenobiotics.
Over the last few decades, over 80,000 industrial chemicals have been produced. These chemicals are ubiquitously present in our daily life. They are used in food supply and consumer products, and also released into the environment, ended up in the air, water, soil, and food chain.1,3,22
Some of these chemical pollutants called persistent organic pollutants (POPs) can persist in the environment for extremely long period of time, for decades and much longer.
The safety of many of these chemicals have not been tested and verified.1,22
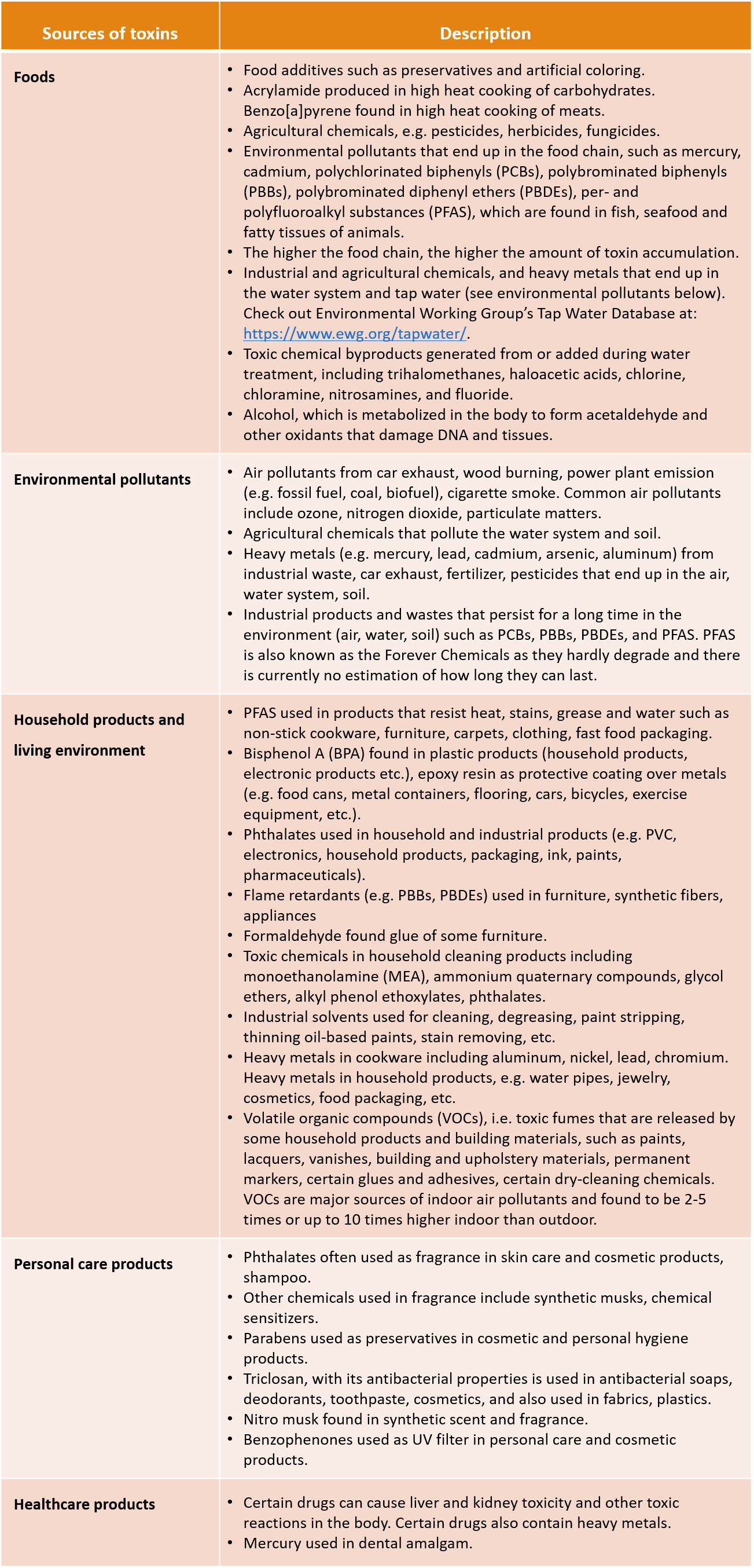
Table 1 below summarizes some common external sources of toxins we are exposed to.
Table 1. Common Sources of Man-made Toxins1,5–21,37,90
The widespread exposure of certain industrial chemicals in our modern living is shown in The Fourth National Report on Human Exposure to Environmental Chemicals (Fourth Report) published by the United States Centers for Disease Control and Prevention (CDC).23
Through measurements of blood and urine samples, chemicals that are widely found among US populations include PBDEs, PBBs, BPA, PFAS, acrylamide, mercury, cadmium, arsenic, methyl tert-butyl ether (MTBE) (a gasoline additive) and perchlorate (used rocket propellant, fireworks, food packaging, etc.).23
Many of the toxins have long half life and stay in the environment for decades and even longer despite some of them may have been discontinued usage due to regulatory policy.
The far reaching effects of toxin exposure in our modern living is also demonstrated by studies of blood or urine samples of pregnant women and umbilical cord blood samples of newborns, which showed the presence of many common industrial chemicals including phthalates, phenols (e.g. BPA, triclosan, parabens), PFAS, flame retardants, PCBs, and organochlorine pesticides (OCs).2–4
Internal Sources of Toxins
Toxins can also be generated internally in our body, usually by pathogens, namely bacteria, parasites and mold.
These internal toxins are called biological toxins or biotoxins, as listed below.
- Ammonia: Ammonia is a normal byproduct of protein metabolism. Ammonia is excreted directly in the urine or converted to urea in the liver before excretion in the urine. In addition to normal protein metabolism, ammonia is also generated by some pathogenic bacteria and parasites. Excess ammonia in the body that cannot be excreted is neurotoxic (causing brain and nervous system damage) and contributes to systemic oxidative stress and inflammation.24–27
- Bacteria toxins: Toxins generated by pathogenic bacteria include endotoxins or lipopolysaccharides (LPS), exotoxins and enterotoxins. LPS is generated by certain pathogenic bacteria in the gut as well as in water-damaged buildings. LPS promotes inflammation in the body including gut inflammation, liver inflammation when LPS is translocated from the gut to the liver, nasal inflammation when exposed to water-damaged building, and systemic uncontrolled inflammatory response or sepsis.28–31
- Mycotoxins: Mycotoxins are toxic chemicals generated by mold. One can acquire mycotoxins externally from water-damaged buildings and foods. Mycotoxins can also be generated internally by mold that grows inside the body. Mycotoxins can be disease causing and in certain cases life threatening.32,33
The Body’s Natural Detoxification Capabilities
Our body has major detoxification capabilities to remove toxins out of the body as described below.
Liver and kidneys are the two major detox organs. Water-soluble toxins are detoxed by the kidneys via urine excretion. Fat-soluble toxins are metabolized in the liver into water-soluble forms and then excreted via bile as part of stool or via urine.
Our gut lining (or intestinal barrier) forms a physical barrier to prevent toxins we ingest from entering the circulatory system. However, when there is aberrancy of the gut lining called intestinal permeability (or leaky gut), toxic compounds “leaked” from the gut lumen to the blood stream and subsequently translocated to the liver.31
Therefore, the health of our gut is also crucial for deterring entry of toxins into our body.
In addition to liver, kidneys and gut, our drainage channels are key to facilitate excretion of toxins out of the body. These drainage channels include:
- Large intestine: Bowel movement facilitate excretion of toxins via stool.
- Bile: Bile (secreted by liver and stored in gallbladder) carries toxins that are metabolized by the liver into the small intestine for subsequent excretion through the large intestine.
- Lymphatic system: Lymphatic system is a major transport system in the body, carrying dietary fats absorbed through the small intestine, immune cells, biological messengers and compounds, metabolic waste and toxins.34
- Skin: Toxins are excreted through our skin when we sweat.
Proper functioning of the above detox organs and drainage channels are key to reduce toxin load in our body.
In our modern living, when we are bombarded with tens of thousands of toxins, the natural detox capabilities of our body can be overwhelmed, resulting in faster rate of toxin acquisition into the body than rate of excretion.1
Toxins not excreted are bio-accumulative in our body, especially in fat tissues, liver, kidneys, bone, and brain, causing chronic health conditions.1
Many of the toxins have long half life and can stay in the body for decades or even longer.38
In the next section, we discuss the adverse health effects of toxins.
How Toxins Affect Our Health?
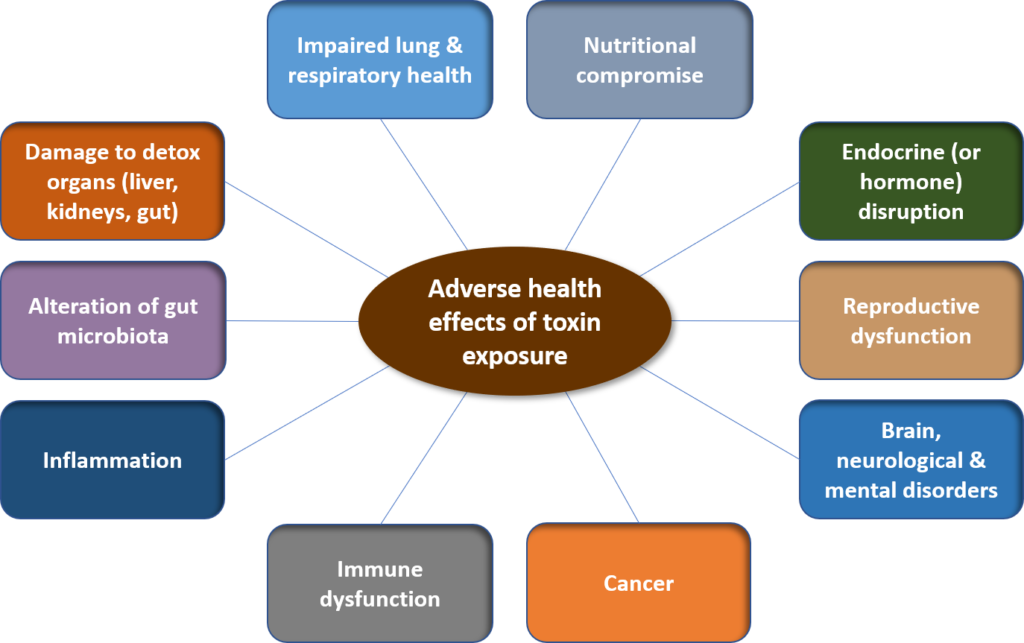
Figure 2. Adverse health effects of toxin exposure
In this section, we focus on the health effects of external or man-made toxins previously described.
Toxic chemicals and metals disrupt normal biochemical and physiological processes and functioning in the body, by the following mechanism:1
- Direct cell damage, alteration of cell function and disruption of cell homeostasis.
- Damage and dysfunction of mitochondria (the energy-making machine in a cell).
- Oxidative stress.
- Alteration of gene expression or epigenetics − induced by some pesticides, insecticides, heavy metals.
- Direct impairment of detoxification function − induced by glyphosate (a widely used herbicide), lead, PBDEs.
- Formation of diseased plagues: 1) Alpha-synucleain found in Parkinson’s disease − induced by some pesticides, metals, solvents; 2) beta-amyloid found in Alzheimer’s disease − induced by lead, mercury, aluminum, cadmium, arsenic, some pesticides; 3) atherosclerotic plaque in heart disease – induced by allylamine, benzo[a]pyrene.
- Displacement of normal binding at cell receptors: e.g. PBDEs displace thyroid hormone T4 binding, cadmium displace zinc binding.
The adverse health effects of the above disruptions are summarized below.
Endocrine (or Hormone) Disruption
Many toxic chemicals are known as endocrine disrupting chemicals (EDCs). They disrupt the endocrine (hormonal) system in two major ways:1
- Amplification effects by mimicking endogenous hormones in the body: For examples, certain toxic chemicals, called xenoestrogens, mimic and exert estrogenic effects in the body, causing estrogen dominant health effects in the body. Examples of xenoestrogens include parabens, phthalates, nitro musk, benzophenones, PCBs, PBBs, BPA, etc.
- Inhibition effects by acting as blocking agent and interfering with hormone excretion, thus disrupting proper delivery to target tissue.
Diseases linked with EDCs are numerous as shown by scientific studies. Here is a brief account:1,35
- Xenoestrogens described above contribute to estrogen dominance in the body. Some diseases associated with estrogen dominance include uterine fibroids, endometriosis, perimenopausal symptoms, PMS, increased risk of certain cancers (incl. breast cancer, endometrial cancer, ovarian cancer, prostate cancer).
- Some EDCs (incl. phthalates, certain fungicides, pesticides) have anti-androgenic effects (suppress male hormones), increasing the risk of congenital abnormalities including cryptorchidism.
- Some EDCs (incl. PCBs, PBBs, PBDEs, phthalates, BPA, PFAS, fluoride) impair thyroid function.
Reproductive Dysfunction
Pre-conception and prenatal exposure to EDCs can affect reproductive health during early pregnancy as well as throughout fetal life. Some of the adverse effects may even be multigenerational.35,36
Some of the adverse effects are listed below.35,36
Phenols (incl. BPA, triclosan, parabens)
- Prenatal exposure to BPA can interfere with fetal neurodevelopment, resulting in increased anxiety, depressive symptoms and impaired behavioral regulation at toddler age, and aggression and hyperactivity in female children.
- BPA exposure reduces male sexual and reproductive function, and promotes recurrent miscarriage.
- Triclosan exposure is associated with reduced thyroid hormone, thyroxine, concentration.
Phthalates
- Phthalate exposure can adversely affect reproduction including poor semen quality and miscarriage.
- Prenatal phthalate exposure is associated with underdevelopment of male reproductive organs and masculine behavior in boys.
- Prenatal phthalate exposure is also associated with poorer cognitive and behavioral outcomes in children, especially boys.
- Phthalate exposure also affects maternal health by increasing the risk of pregnancy-induced hypertensive disorders and reducing gestational age.
PBDEs
- Prenatal exposure to PBDEs affects fetal neurodevelopment, resulting in impaired attention, lower IQ, poorer fine motor coordination in offspring at age 5 to 7.
PFAS
- Exposure to PFAS is associated with reduced fecundity and infertility in women.
- Prenatal PFAS exposure is associated with poorer fetal growth, reduced birthweight and increased risk of thyroid disease in children.
- PFAS exposure also affects maternal health by increasing the risk of pregnancy-induced hypertensive disorders.
PCBs
- Exposure to PCBs can decrease semen quality.
- Prenatal PCB exposure results in low birth weight, reduced IQ, attention deficit hyperactivity disorder (ADHD) in offspring.
Heavy metals (incl. cadmium, lead, mercury)
- Prenatal exposure results in epigenetic alteration of the placenta and newborns, and impaired neurodevelopment (incl. decreased cognitive function and IQ, increased incidence of behavioral problems, reduced psychomotor outcomes) in offspring.
Perchlorate
- Prenatal exposure alters thyroid function in newborns.
Solvents
- Maternal exposure is associated with spontaneous abortion and fetal loss, decreased fetal and birthweight and congenital malformations.
Pesticides
- Prenatal exposure impairs fetal growth, impairs neurodevelopment (incl. decreased cognitive function and IQ, increased risk of pervasive development disorder and ADHD).
- Prenatal exposure also increased susceptibility to testicular cancer and other childhood cancers (incl. leukemia, brain tumor) in offspring.
- to organophosphate pesticides is associated with poorer IQ in offspring children.
Brain, Neurological and Mental Disorders
Many toxins are neurotoxic and have neurodegenerative effects, causing dysfunction and death of neurons, which can have cognitive, mental and physical consequences.38–43
Some common neurodegenerative diseases include Alzheimer’s disease, Parkinson’s disease, Multiple Sclerosis (MS), and Amyotrophic Lateral Sclerosis (ALS).
Here is a brief summary toxins implicated in the increased incidence of certain neurodegenerative and neurodevelopmental diseases:38–43,96
- Alzheimer’s disease, dementia and cognitive decline: Exposure to PBDEs, pesticides/herbicides, heavy metals (incl. lead, mercury, aluminum, arsenic, cadmium), air pollutants (incl. ozone, particulate matter, nitrogen dioxide).
- Parkinson’s disease: Exposure to lead, pesticides/herbicides/fungicides, solvents.
- ALS: Exposure to lead, mercury, pesticides.
- MS: Exposure to solvents.
- Autism Spectrum Disorder: Exposure to mercury, lead, pesticides, air pollutants (incl. particulate matters, nitrogen dioxide, ozone).
Exposure to air pollutants, pesticides, lead is associated with poor mental health.91,95,96
In addition, exposure that occurs early in life when brain and nervous system are still developing, can have more profound effects.96
Cancer
Many toxins we are exposed to in modern living are carcinogens, which can cause altered gene expression, DNA damage and mutation, oxidative stress, mitochondria dysfunction, hormonal disruption; all of which are contributing factors to the disease process of cancer.1
A comprehensive list of known and probable human carcinogens and affected organs/tissues, published by the World Health Organization can be found here.44
Some of the common ones include PCBs, PBBs, PFAS, arsenic, lead, chromium, nickel, cadmium, tobacco smoke, smokeless tobacco, air pollutants, formaldehyde, glyphosate, acrylamide, benzo[a]pyrene, processed meat and red meat, contraceptives, hormone replacement therapy, acetaldehyde (from alcohol metabolism), and some drugs.44,90
Immune Dysfunction
Toxins can dysregulate immune system resulting in immune suppression, autoimmune disorders and hypersensitivity.1
Heavy metals such as mercury and pesticides, can suppress immune defense.1
Exposure to solvents, pesticides, heavy metals can trigger autoimmune response.1
Immune hypersensitivity can manifest into allergic reactions or environmental sensitivities (also called multiple chemical sensitivities). For example, exposure to solvents is associated with MS, while exposure to solvents, pesticides, heavy metals, air pollutants, cigarette smoke, crystalline silica is associated with systemic lupus erythematosus (SLE). 1,38,45
Prenatal exposure to toxins can predispose offspring to pediatric allergies and hypersensitivity. Prenatal exposure to PCBs, dioxin, PFCs, lead, polycyclic aromatic hydrocarbons (PAHs) is associated with respiratory symptoms and other allergies in newborn and children.1
Inflammation
Toxins can trigger inflammation through various mechanisms including directly triggering release of pro-inflammatory signaling, or indirectly promoting oxidative stress and cellular damage resulting in inflammation.1
On-going assault of toxins can result in chronic oxidative stress and chronic systemic inflammation, which in turn are major culprits and underlying disease process of many chronic diseases/disorders that are becoming increasingly prevalent including type 2 diabetes, hypertension, heart disease, obesity, Alzheimer’s disease, cancer, etc.46–50,94
Alteration of Gut Microbiota
Gut microbiota is the ecology is microorganisms (bacteria, viruses, parasites, fungi, etc.) in the gut. Microorganisms can be good (symbiotic), bad (pathogenic) or commensal.
Symbiotic microbiota play important roles in the health of human host, not only digestion and gut health, but also immune health, brain health, synthesis and metabolism of certain nutrients, etc.51–53
Exposure to toxins including heavy metals (incl. arsenic, cadmium, cobalt, chromium, nick, lead), pesticides, nanoparticles, PAHs, dioxins, furans, PCBs, air pollutants, non-caloric artificial sweeteners, chronic alcohol consumption, and antibiotics alters gut microbiota, which in turns contribute to the development of metabolic disorders/diseases (e.g. obesity, type 2 diabetes, high LDL/low HDL cholesterol, heart disease), gut dysfunction/disorders, cancer, chronic liver diseases, chronic kidney disease, immune and inflammatory diseases.54–56
For more information on gut and gut microbiota health, please check out my previous articles: “Why Your Gut Feeling Matters”, “You Are What You Eat? Not Quite”, “Tips to Promote Gut Health for a Healthy Body & Mind”.
Damage to Detox Organs (Liver, Kidneys, Gut)
Our liver, kidneys and gut are the frontline detox organs that defend against toxins circulating in the rest of the body.
These organs are vulnerable to the direct assault of toxins that leads to tissue damage and dysfunction, which in turn degrades the overall detoxification ability of the body.
Liver
Chronic exposure to toxic chemicals throughout the lifetime increases the risk of liver injury and promotes liver disease later in life.57
The detrimental effects can start as early as during the gestational period (i.e. in the mother’s womb) if the mother is exposed to toxic chemicals during pregnancy.57
Liver disease caused by exposures to chemicals has been termed “toxicant-associated fatty liver disease”.57,58
Some toxic chemicals associated with chronic liver disease include pesticides/herbicides/insecticides/fungicides, solvents, PCBs, paints/polishes/dyes, chemicals found is fragrance and cosmetics, EDCs, tobacco smoke, some drugs, and heavy metals (incl. arsenic, cadmium, chromium, copper, lead, mercury).58–64
Kidneys
Many toxins including solvents, pesticides/herbicides, heavy metals (incl. lead, mercury, cadmium, copper, uranium), fluoride, tobacco smoke, air pollutants, certain drugs (incl. certain antibiotics, antiviral drugs, chemotherapeutic drugs, immunosuppressive drugs, NSAIDs, proton pump inhibitors, bisphosphonates, analgesic) are toxic to the kidneys, causing acute tissue injury and damage and chronic kidney disease.65–68
Toxin exposure if also implicated in pediatric kidney disease among children.69
Gut
Exposure to toxins including certain drugs (NSAIDs, antibiotics, proton pump inhibitors, anticancer therapy), air pollutants, PCBs, glyphosate, heavy metals (incl. aluminum, cadmium, mercury) and alcohol, can impair and degrade the gut lining, contributing to intestinal permeability (or leaky gut) and intestinal inflammation.70–77,90
In addition, dysbiosis (imbalance of gut microbiota) also contributes to intestinal permeability.78
When the gut lining becomes ‘leaky’, unwanted substances that we ingest into the gut or biotoxins generated by microorganisms in the gut can be translocated to other parts of the body.
Intestinal permeability is implicated in a wide range of chronic diseases, including inflammatory bowel disease, irritable bowel syndrome, celiac disease, non-celiac gluten sensitivity, food allergies and sensitivities, obesity and other metabolic disorders, autoimmune disorders, brain, neurological and mental disorders.76–79
Because of translocation of biotoxin and xenobiotics from the gut lumen to the detox organs, i.e. liver and kidneys, intestinal permeability can also contribute to chronic liver disease and chronic kidney disease.78,79
Impaired Lung and Respiratory Health
Our respiratory tract and lung are in direct contact with pollutants in the air we breathe in.
Exposure to air pollutants triggers oxidative stress and inflammation in the respiratory tract and lung, and is linked to exacerbation of pre-existing lung disease, development of respiratory infections, chronic obstructive pulmonary disease (COPD), pulmonary fibrosis, asthma, and allergic inflammation.89
Nutritional Compromise
As discussed above, toxin exposure can compromise gut health, thus affecting digestion and absorption.
For example, tobacco smoking is associated with reduced levels of vitamins B6, C and E, folic acid, beta carotene and zinc.1
Toxins also affect metabolism of certain nutrients in the body. Cadmium decreases intestinal absorption of calcium, impairs vitamin D activation in the kidneys and increases calcium excretion through the urine, thus affecting bone health.1
In addition to cadmium, lead and chromium also affect bone metabolism, contributing to loss of bone mass and osteoporosis.80
Certain drugs can contribute to nutritional deficiency. For example, antacids are linked to deficiency of folic acid, calcium, copper, phosphate, vitamins A and B12. Antibiotics are linked to deficiency of vitamin D, L-leucine and biotin. Oral contraceptives are linked to deficiency of magnesium, manganese, zinc, folic acid, vitamins B1, B2, B3, B6, B12 and C.1
Tips to Reduce Toxic Load in the Body
It is always better to prevent toxins from entering our body rather than removing the toxins after they have entered the body.
Therefore, minimize toxin exposure is of utmost importance.
Even if we try our best, we still cannot avoid toxin exposure as toxins are so ubiquitous in our living environment. Therefore, we need to support our detox organs and drainage channels in excreting toxins that have entered our body.
Throughout our lifetime, there are likely numerous toxins that have bio-accumulated in our body. Toxins that are chronically bio-accumulated deep in the tissues and cells for a long period of time may require some specific detox protocol to facilitate removal.
The following sections provide some tips on different aspects of reducing toxic load in our body.
Minimize Toxin Exposure
As discussed in section External Sources of Toxins, there are many sources of toxins. Once we know these sources, we can try to avoid them. Here is a list of recommendations.
Eat Clean Foods
- Consume organic foods whenever possible, or at least choose organic for those produce that is known to be laden with pesticides/herbicides etc.
- Check out Environmental Working Group’s (EWG) shopper’s guide at: https://www.ewg.org/foodnews/.
- Avoid high heat cooking which can produce toxic chemicals.
Eat Whole Foods
- Minimize consumption of processed foods which are often filled with food chemicals and additives.
- When buying processed or packaged food products, always check the label for ingredients and avoid those that have non-food ingredients.
Eat Lower in the Food Chain
- Eat a whole food plant-rich diet as toxins tend to accumulate higher in the food chain, especially fatty tissues in animals.
- A whole food plant-rich diet is high anti-oxidative and anti-inflammatory compounds that help to combat oxidative stress incurred by toxins in the body.
- Avoid fish that tend to be high in mercury, including swordfish, marlin, king mackerel, orange roughy, etc. Check out EWG’s seafood guide at: https://www.ewg.org/research/ewgs-good-seafood-guide.
- Choose meats that are organic and grass-fed/pasture-raised that is free of antibiotics and lower in toxic chemical accumulation.
Drink Clean Water
- Filter your tap water – check out EWG’s water filter guide at: https://www.ewg.org/tapwater/water-filter-guide.php.
- Bottled water may not be the solution as many popular brands of bottled water may be contaminated with toxic chemicals. Chemicals may also leach from the plastic bottles.81
Choose Clean Personal Care and Household Cleaning Products
- Natural personal care and household cleaning products are usually better.
- Always check the label for ingredients and avoid products that have known toxic chemicals and metals.
- For personal care products, check out EWG’s guide at: https://www.ewg.org/skindeep/.
- For household cleaning products, check out EWG’s guide at: https://www.ewg.org/guides/cleaners/.
Clean Your Indoor Air
- Indoor air can be 2-5 times or as high as 10 times worse in VOCs pollution than outdoor air due to VOCs leaching from furniture, building materials, household products, etc.
- Use an air purifier at home that has high-grade HEPA filter.
- You may go one step further by choosing low-toxicity furniture and building supplies.
- Check out EWG’s home guide at: https://www.ewg.org/healthyhomeguide/.
Choose Cleaner Cookware and Utensils
- Avoid aluminum cookware and utensils including aluminum foil.
- Avoid plastic containers, utensils, etc. as much as possible.
- Avoid Teflon cookware. Even ceramic-coated non-stick cookware can leach heavy metals when scratched.
- Glass, 100% ceramic and stainless steel cookware are relatively safer and better choice. Choose high-grade stainless steel appliances, e.g. 304 or higher. However, beware not to scratch the surface lining of stainless steel cookware as the internal heavy metals (incl chromium, nickel; some stainless steel cookware also contains aluminum) can leach out. Cooking acidic foods in stainless steel cookware also promote leaching of heavy metals.
- Cast iron cookware may not be bad however excess iron in the body can lead to adverse health effects. Men and postmenopausal women are at higher risk of excess iron.
- Similarly, copper cookware can increase the risk of excess copper in the body causing adverse health effects.
Support Detox Organs and Drainage Channels in the Body
By minimizing toxin exposure to the body as discussed above, we can also minimize direct assault of toxins and potential damage to our detox organs.
In addition, we should also support the health of our detox organs and drainage channels through adequate diet and lifestyle choices as follows.
Support Liver Health
- A whole food plant-rich diet that is high in anti-oxidative and anti-inflammatory properties are beneficial for liver health.
- In addition, consume probiotic and prebiotic rich foods, avoid added sugars and sweeteners and avoid excessive alcohol consumption.
- Lifestyle strategies to promote liver health include adequately manage stress, ensure adequate sleep, maintain healthy weight, support healthy vitamin D levels, and avoid cigarette smoking.
- For more details on tips to support liver health, check out my previous article: “Take Care of Your Liver for Healthy Immunity and Overall Wellness”.
Support Gut Health
- In addition to the above strategies for liver health, it is also important to avoid foods that trigger immune reactions and inflammation, i.e., food allergies and hidden food sensitivities.
- Address deeply rooted and hidden gut dysfunctions which can often go undiagnosed or unrecognized, including gut infections, leaky gut, and gut inflammation. Some deep-dive investigation such as functional lab testing may be necessary.
- For more details on tips to support gut health, please check out my previous article: “Tips to Promote Gut Health for a Healthy Body & Mind”.
- For additional support in addressing hidden food sensitivities and deeply rooted gut issues, please check out Functional Health Coaching.
Support Kidney Health
- Besides toxin exposure, common risk factors of chronic kidney disease include hypertension, type 2 diabetes, obesity, dyslipidemia (elevated triglyceride, LDL cholesterol, total cholesterol) and chronic liver disease.82
- One common underlying culprit of these chronic diseases is oxidative stress and chronic inflammation.
- Diet and lifestyle choices play important roles. In addition to the above recommended strategies for liver and gut health, please check out my article series: “Diets and Chronic Diseases”.
Support the Health of Drainage Channels
- Support gut health as discussed above to ensure health bowel movement.
- Support regular sweating through physical exercise and sauna.
- Support healthy bile flow by supporting liver and gallbladder health using strategies as discussed above.
- Support lymphatic drainage through healthy dietary strategies discussed above, and also physical movement and exercise, dry skin brushing, lymphatic drainage massage, deep breathing, infrared sauna, and adequate sleep (which is crucial for the drainage of brain lymphatic, also called glymphatic system).83–87
- Drink plenty of clean water to facilitate transport of toxins in lymph, sweat and urine. A simple guideline for the amount of water to consume is to make sure the urine excreted has clear, pale yellow color instead of dark yellow/brown color.
Employ Specific Detox Protocol
While adopting a healthy diet and lifestyle strategies as discussed above is important, some time we may need extra support for our detox organs and drainage channels (incl. liver and bile, kidneys, gut, lymphatic system) since there may already be some dysfunction going on in these organs due to chronic toxin accumulation, chronic infections, unhealthy diet and lifestyle in the past, etc.
In addition, when toxins are bio-accumulated deep inside tissues and cells, some specific detox protocol may be needed to pull toxins out for excretion out of the body.
Components of a detox protocol may include:
- Specific protocol (e.g. coffee enema, lemon water, cleansing diet, etc.) and supplements (e.g., nutritional, herbal) to provide extra support to detox organs and drainage channels (incl. liver and bile, kidneys, gut, lymphatic system).
- Specific protocol (e.g. infrared sauna, fasting, etc.) and supplements (e.g., nutritional, herbal) to mobilize, chelate and bind toxins for excretion out of the body.
- Addressing deeply rooted issues that promote the body holding on to toxins. For example, parasites may sequester toxins especially heavy metals in the host body.88 Therefore, a detox protocol may also involve parasite cleansing.
Since each person’s health conditions and challenges are unique, detox protocol should be individualized.
Related Articles
You are What You Eat? Not Quite
Tips to Promote Gut Health for a Healthy Body & Mind
Take Care of Your Liver for Healthy Immunity and Overall Wellness
References
-
- Genuis SJ, Kyrillos E. The chemical disruption of human metabolism. Toxicol Mech Methods. 2017;27(7):477-500. doi:10.1080/15376516.2017.1323986
- Woodruff TJ, Zota AR, Schwartz JM. Environmental chemicals in pregnant women in the United States: NHANES 2003-2004. Environ Health Perspect. 2011;119(6):878-885. doi:10.1289/ehp.1002727
- Mitro SD, Johnson T, Zota AR. Cumulative Chemical Exposures During Pregnancy and Early Development. Curr Environ Health Rep. 2015;2(4):367-378. doi:10.1007/s40572-015-0064-x
- Environmental Working Group. Body Burden: The Pollution in Newborns. EWG. https://www.ewg.org/research/body-burden-pollution-newborns. Published 2005.
- Li Y, Zhou Q, Ren B, et al. Trends and Health Risks of Dissolved Heavy Metal Pollution in Global River and Lake Water from 1970 to 2017. Rev Environ Contam Toxicol. 2020;251:1-24. doi:10.1007/398_2019_27
- Pelch KE, Reade A, Wolffe TAM, Kwiatkowski CF. PFAS health effects database: Protocol for a systematic evidence map. Environ Int. 2019;130:104851. doi:10.1016/j.envint.2019.05.045
- United States Environmental Protection Agency. Basic Information on PFAS. US EPA. https://www.epa.gov/pfas/basic-information-pfas.
- Environmental Protection Agency. https://www.epa.gov/.
- Environmental Working Group. https://www.ewg.org/.
- Campaign for Safe Cosmetics. http://www.safecosmetics.org/.
- Al-Eryani L, Wahlang B, Falkner KC, et al. Identification of Environmental Chemicals Associated with the Development of Toxicant-associated Fatty Liver Disease in Rodents. Toxicol Pathol. 2015;43(4):482-497. doi:10.1177/0192623314549960
- Teschke R. Top-ranking drugs out of 3312 drug-induced liver injury cases evaluated by the Roussel Uclaf Causality Assessment Method. Expert Opin Drug Metab Toxicol. 2018;14(11):1169-1187. doi:10.1080/17425255.2018.1539077
- Teschke R. Idiosyncratic DILI: Analysis of 46,266 Cases Assessed for Causality by RUCAM and Published From 2014 to Early 2019. Front Pharmacol. 2019;10:730. Published 2019 Jul 23. doi:10.3389/fphar.2019.00730
- Guengerich FP. Mechanisms of drug toxicity and relevance to pharmaceutical development. Drug Metab Pharmacokinet. 2011;26(1):3-14. doi:10.2133/dmpk.dmpk-10-rv-062
- Guarneri F, Costa C, Cannavò SP, et al. Release of nickel and chromium in common foods during cooking in 18/10 (grade 316) stainless steel pots. Contact Dermatitis. 2017;76(1):40-48. doi:10.1111/cod.12692
- Homme KG, Kern JK, Haley BE, et al. New science challenges old notion that mercury dental amalgam is safe. Biometals. 2014;27(1):19-24. doi:10.1007/s10534-013-9700-9
- Wells EM, Kopylev L, Nachman R, Radke EG, Segal D. Seafood, wine, rice, vegetables, and other food items associated with mercury biomarkers among seafood and non-seafood consumers: NHANES 2011-2012. J Expo Sci Environ Epidemiol. 2020;30(3):504-514. doi:10.1038/s41370-020-0206-6
- Environmental Working Group. The Dirty Secret of Government Drinking Water Standards. Ewg.org. https://www.ewg.org/tapwater/state-of-american-drinking-water.php. Published 2020.
- Environmental Working Group. Water Treatment Contaminants:. EWG. https://www.ewg.org/research/water-treatment-contaminants. Published 2013.
- Malin AJ, Lesseur C, Busgang SA, Curtin P, Wright RO, Sanders AP. Fluoride exposure and kidney and liver function among adolescents in the United States: NHANES, 2013-2016. Environ Int. 2019;132:105012. doi:10.1016/j.envint.2019.105012
- Green R, Lanphear B, Hornung R, et al. Association Between Maternal Fluoride Exposure During Pregnancy and IQ Scores in Offspring in Canada [published online ahead of print, 2019 Aug 19]. JAMA Pediatr. 2019;173(10):940-948. doi:10.1001/jamapediatrics.2019.1729
- Wang A, Padula A, Sirota M, Woodruff TJ. Environmental influences on reproductive health: the importance of chemical exposures. Fertil Steril. 2016;106(4):905-929. doi:10.1016/j.fertnstert.2016.07.1076
- Centers for Disease Control and Prevention. National Report on Human Exposure to Environmental Chemicals. Cdc.gov. https://www.cdc.gov/exposurereport/index.html. Published 2019.
- Weiner ID, Mitch WE, Sands JM. Urea and Ammonia Metabolism and the Control of Renal Nitrogen Excretion. Clin J Am Soc Nephrol. 2015;10(8):1444-1458. doi:10.2215/CJN.10311013
- Kimoloi S, Rashid K. Potential role of Plasmodium falciparum-derived ammonia in the pathogenesis of cerebral malaria. Front Neurosci. 2015;9:234. Published 2015 Jul 3. doi:10.3389/fnins.2015.00234
- Richardson AJ, McKain N, Wallace RJ. Ammonia production by human faecal bacteria, and the enumeration, isolation and characterization of bacteria capable of growth on peptides and amino acids. BMC Microbiol. 2013;13:6. Published 2013 Jan 11. doi:10.1186/1471-2180-13-6
- Mancini A, Campagna F, Amodio P, Tuohy KM. Gut : liver : brain axis: the microbial challenge in the hepatic encephalopathy. Food Funct. 2018;9(3):1373-1388. doi:10.1039/c7fo01528c
- Ramachandran G. Gram-positive and gram-negative bacterial toxins in sepsis: a brief review. Virulence. 2014;5(1):213-218. doi:10.4161/viru.27024
- Akpinar-Elci M, White SK, Siegel PD, et al. Markers of upper airway inflammation associated with microbial exposure and symptoms in occupants of a water-damaged building. Am J Ind Med. 2013;56(5):522-530. doi:10.1002/ajim.22165
- Park J, Lee IS, Kim KH, Kim Y, An EJ, Jang HJ. GI inflammation Increases Sodium-Glucose Cotransporter Sglt1. Int J Mol Sci. 2019;20(10):2537. Published 2019 May 23. doi:10.3390/ijms20102537
- Albhaisi SAM, Bajaj JS, Sanyal AJ. Role of gut microbiota in liver disease. Am J Physiol Gastrointest Liver Physiol. 2020;318(1):G84-G98. doi:10.1152/ajpgi.00118.2019
- Bennett JW, Klich M. Mycotoxins. Clin Microbiol Rev. 2003;16(3):497-516. doi:10.1128/cmr.16.3.497-516.2003
- Brewer JH, Thrasher JD, Hooper D. Chronic illness associated with mold and mycotoxins: is naso-sinus fungal biofilm the culprit?. Toxins (Basel). 2013;6(1):66-80. Published 2013 Dec 24. doi:10.3390/toxins6010066
- Goswami AK, Khaja MS, Downing T, Kokabi N, Saad WE, Majdalany BS. Lymphatic Anatomy and Physiology. Semin Intervent Radiol. 2020;37(3):227-236. doi:10.1055/s-0040-1713440
- Zlatnik MG. Endocrine-Disrupting Chemicals and Reproductive Health. J Midwifery Womens Health. 2016;61(4):442-455. doi:10.1111/jmwh.12500
- Wang A, Padula A, Sirota M, Woodruff TJ. Environmental influences on reproductive health: the importance of chemical exposures. Fertil Steril. 2016;106(4):905-929. doi:10.1016/j.fertnstert.2016.07.1076
- Tsai WT. An overview of health hazards of volatile organic compounds regulated as indoor air pollutants. Rev Environ Health. 2019;34(1):81-89. doi:10.1515/reveh-2018-0046
- Genuis SJ, Kelln KL. Toxicant exposure and bioaccumulation: a common and potentially reversible cause of cognitive dysfunction and dementia. Behav Neurol. 2015;2015:620143. doi:10.1155/2015/620143
- Cannon JR, Greenamyre JT. The role of environmental exposures in neurodegeneration and neurodegenerative diseases. Toxicol Sci. 2011;124(2):225-250. doi:10.1093/toxsci/kfr239
- Chin-Chan M, Navarro-Yepes J, Quintanilla-Vega B. Environmental pollutants as risk factors for neurodegenerative disorders: Alzheimer and Parkinson diseases. Front Cell Neurosci. 2015;9:124. Published 2015 Apr 10. doi:10.3389/fncel.2015.00124
- Chun H, Leung C, Wen SW, McDonald J, Shin HH. Maternal exposure to air pollution and risk of autism in children: A systematic review and meta-analysis. Environ Pollut. 2020;256:113307. doi:10.1016/j.envpol.2019.113307
- Rossignol DA, Genuis SJ, Frye RE. Environmental toxicants and autism spectrum disorders: a systematic review. Transl Psychiatry. 2014;4(2):e360. Published 2014 Feb 11. doi:10.1038/tp.2014.4
- Saghazadeh A, Rezaei N. Systematic review and meta-analysis links autism and toxic metals and highlights the impact of country development status: Higher blood and erythrocyte levels for mercury and lead, and higher hair antimony, cadmium, lead, and mercury. Prog Neuropsychopharmacol Biol Psychiatry. 2017;79(Pt B):340-368. doi:10.1016/j.pnpbp.2017.07.011
- International Agency for Research on Cancer, World Health Organization. IARC Monographs on the Identification of Carcinogenic Hazards to Humans. Monographs.iarc.fr. https://monographs.iarc.fr/agents-classified-by-the-iarc/. Published 2020.
- Parks CG, de Souza Espindola Santos A, Barbhaiya M, Costenbader KH. Understanding the role of environmental factors in the development of systemic lupus erythematosus. Best Pract Res Clin Rheumatol. 2017;31(3):306-320. doi:10.1016/j.berh.2017.09.005
- Esser N, Legrand-Poels S, Piette J, Scheen A, Paquot N. Inflammation as a link between obesity, metabolic syndrome and type 2 diabetes. Diabetes Res Clin Pract. 2014;105(2):141-150. doi:10.1016/j.diabres.2014.04.006
- Golia E, Limongelli G, Natale F et al. Inflammation and Cardiovascular Disease: From Pathogenesis to Therapeutic Target. Curr Atheroscler Rep. 2014;16(9). doi:10.1007/s11883-014-0435-z
- Newcombe E, Camats-Perna J, Silva M, Valmas N, Huat T, Medeiros R. Inflammation: the link between comorbidities, genetics, and Alzheimer’s disease. J Neuroinflammation. 2018;15(1). doi:10.1186/s12974-018-1313-3
- Moss S, Blaser M. Mechanisms of Disease: inflammation and the origins of cancer. Nature Clinical Practice Oncology. 2005;2(2):90-97. doi:10.1038/ncponc0081
- Murata M. Inflammation and cancer. Environ Health Prev Med. 2018;23(1). doi:10.1186/s12199-018-0740-1
- Morowitz MJ, Carlisle EM, Alverdy JC. Contributions of intestinal bacteria to nutrition and metabolism in the critically ill. Surg Clin North Am. 2011;91(4):771-85, viii.
- Quigley EMM. Gut bacteria in health and disease. Gastroenterol Hepatol (N Y). 2013;9(9):560-9.
- Mirjana R. Function of the microbiota. Best Pract Res Clin Gastroenterol. 2013;27(1):5-16. doi:10.1016/j.bpg.2013.03.006
- Tsiaoussis J, Antoniou MN, Koliarakis I, et al. Effects of single and combined toxic exposures on the gut microbiome: Current knowledge and future directions. Toxicol Lett. 2019;312:72-97. doi:10.1016/j.toxlet.2019.04.014
- Koontz JM, Dancy BCR, Horton CL, Stallings JD, DiVito VT, Lewis JA. The Role of the Human Microbiome in Chemical Toxicity. Int J Toxicol. 2019;38(4):251-264. doi:10.1177/1091581819849833
- Fouladi F, Bailey MJ, Patterson WB, et al. Air pollution exposure is associated with the gut microbiome as revealed by shotgun metagenomic sequencing. Environ Int. 2020;138:105604. doi:10.1016/j.envint.2020.105604
- Treviño LS, Katz TA. Endocrine Disruptors and Developmental Origins of Nonalcoholic Fatty Liver Disease. Endocrinology. 2018;159(1):20-31. doi:10.1210/en.2017-00887
- Al-Eryani L, Wahlang B, Falkner KC, et al. Identification of Environmental Chemicals Associated with the Development of Toxicant-associated Fatty Liver Disease in Rodents. Toxicol Pathol. 2015;43(4):482-497. doi:10.1177/0192623314549960
- Heindel JJ, Blumberg B, Cave M, et al. Metabolism disrupting chemicals and metabolic disorders. Reprod Toxicol. 2017;68:3-33. doi:10.1016/j.reprotox.2016.10.001
- Foulds CE, Treviño LS, York B, Walker CL. Endocrine-disrupting chemicals and fatty liver disease. Nat Rev Endocrinol. 2017;13(8):445-457. doi:10.1038/nrendo.2017.42
- Teschke R. Top-ranking drugs out of 3312 drug-induced liver injury cases evaluated by the Roussel Uclaf Causality Assessment Method. Expert Opin Drug Metab Toxicol. 2018;14(11):1169-1187. doi:10.1080/17425255.2018.1539077
- Teschke R. Idiosyncratic DILI: Analysis of 46,266 Cases Assessed for Causality by RUCAM and Published From 2014 to Early 2019. Front Pharmacol. 2019;10:730. Published 2019 Jul 23. doi:10.3389/fphar.2019.00730
- García-Niño WR, Pedraza-Chaverrí J. Protective effect of curcumin against heavy metals-induced liver damage. Food Chem Toxicol. 2014;69:182-201. doi:10.1016/j.fct.2014.04.016
- Liu Y, Dai M, Bi Y, et al. Active smoking, passive smoking, and risk of nonalcoholic fatty liver disease (NAFLD): a population-based study in China. J Epidemiol. 2013;23(2):115-121. doi:10.2188/jea.je20120067
- George B, You D, Joy MS, Aleksunes LM. Xenobiotic transporters and kidney injury. Adv Drug Deliv Rev. 2017;116:73-91. doi:10.1016/j.addr.2017.01.005
- Dharmaratne RW. Exploring the role of excess fluoride in chronic kidney disease: A review. Hum Exp Toxicol. 2019;38(3):269-279. doi:10.1177/0960327118814161
- Hosohata K. Role of Oxidative Stress in Drug-Induced Kidney Injury. Int J Mol Sci. 2016;17(11):1826. Published 2016 Nov 1. doi:10.3390/ijms17111826
- Xu X, Nie S, Ding H, Hou FF. Environmental pollution and kidney diseases. Nat Rev Nephrol. 2018;14(5):313-324. doi:10.1038/nrneph.2018.11
- Zheng LY, Sanders AP, Saland JM, Wright RO, Arora M. Environmental exposures and pediatric kidney function and disease: A systematic review. Environ Res. 2017;158:625-648. doi:10.1016/j.envres.2017.06.029
- Tinkov AA, Gritsenko VA, Skalnaya MG, Cherkasov SV, Aaseth J, Skalny AV. Gut as a target for cadmium toxicity. Environ Pollut. 2018;235:429-434. doi:10.1016/j.envpol.2017.12.114
- Vignal C, Desreumaux P, Body-Malapel M. Gut: An underestimated target organ for Aluminum. Morphologie. 2016;100(329):75-84. doi:10.1016/j.morpho.2016.01.003
- Vázquez M, Vélez D, Devesa V. In vitro evaluation of inorganic mercury and methylmercury effects on the intestinal epithelium permeability. Food Chem Toxicol. 2014;74:349-359. doi:10.1016/j.fct.2014.10.022
- Melichar B, Zezulová M. The significance of altered gastrointestinal permeability in cancer patients. Curr Opin Support Palliat Care. 2011;5(1):47-54. doi:10.1097/SPC.0b013e328343a043
- Choi YJ, Seelbach MJ, Pu H, et al. Polychlorinated biphenyls disrupt intestinal integrity via NADPH oxidase-induced alterations of tight junction protein expression. Environ Health Perspect. 2010;118(7):976-981. doi:10.1289/ehp.0901751
- Meftaul IM, Venkateswarlu K, Dharmarajan R, et al. Controversies over human health and ecological impacts of glyphosate: Is it to be banned in modern agriculture?. Environ Pollut. 2020;263(Pt A):114372. doi:10.1016/j.envpol.2020.114372
- König J, Wells J, Cani PD, et al. Human Intestinal Barrier Function in Health and Disease. Clin Transl Gastroenterol. 2016;7(10):e196. Published 2016 Oct 20. doi:10.1038/ctg.2016.54
- Bischoff SC, Barbara G, Buurman W, et al. Intestinal permeability–a new target for disease prevention and therapy. BMC Gastroenterol. 2014;14:189. Published 2014 Nov 18. doi:10.1186/s12876-014-0189-7
- Camilleri M. Leaky gut: mechanisms, measurement and clinical implications in humans. Gut. 2019;68(8):1516-1526. doi:10.1136/gutjnl-2019-318427
- Fukui H. Increased Intestinal Permeability and Decreased Barrier Function: Does It Really Influence the Risk of Inflammation?. Inflamm Intest Dis. 2016;1(3):135-145. doi:10.1159/000447252
- Scimeca M, Feola M, Romano L, et al. Heavy metals accumulation affects bone microarchitecture in osteoporotic patients. Environ Toxicol. 2017;32(4):1333-1342. doi:10.1002/tox.22327
- Environmental Working Group. Top 5 Reasons to Choose Filters Over Bottled Water. Ewg.org. https://www.ewg.org/tapwater/bottled-water-resources.php. Published 2019.
- Marcuccilli M, Chonchol M. NAFLD and Chronic Kidney Disease. Int J Mol Sci. 2016;17(4):562. Published 2016 Apr 14. doi:10.3390/ijms17040562
- Nash G. The Lymphatic System: A Critical Factor in Female Hormonal Balance. Ndnr. http://ndnr.com/womens-health/the-lymphatic-system-a-critical-factor-in-female-hormonal-balance. Published 2018.
- Jessen NA, Munk AS, Lundgaard I, Nedergaard M. The Glymphatic System: A Beginner’s Guide. Neurochem Res. 2015;40(12):2583-2599. doi:10.1007/s11064-015-1581-6
- Inoue K, Maruoka H. Effects of simplified lymph drainage on the body: in females with menopausal disorder. J Phys Ther Sci. 2017;29(1):115-118. doi:10.1589/jpts.29.115
- Schwartz N, Chalasani MLS, Li TM, Feng Z, Shipman WD, Lu TT. Lymphatic Function in Autoimmune Diseases. Front Immunol. 2019;10:519. Published 2019 Mar 20. doi:10.3389/fimmu.2019.00519
- Li K, Zhang Z, Liu NF, et al. Efficacy and safety of far infrared radiation in lymphedema treatment: clinical evaluation and laboratory analysis. Lasers Med Sci. 2017;32(3):485-494. doi:10.1007/s10103-016-2135-0
- Sures B, Nachev M, Selbach C, Marcogliese DJ. Parasite responses to pollution: what we know and where we go in ‘Environmental Parasitology’. Parasit Vectors. 2017;10(1):65. Published 2017 Feb 6. doi:10.1186/s13071-017-2001-3
- Losacco C, Perillo A. Particulate matter air pollution and respiratory impact on humans and animals. Environ Sci Pollut Res Int. 2018;25(34):33901-33910. doi:10.1007/s11356-018-3344-9
- Rusyn I, Bataller R. Alcohol and toxicity. J Hepatol. 2013;59(2):387-388. doi:10.1016/j.jhep.2013.01.035
- Klompmaker JO, Hoek G, Bloemsma LD, et al. Associations of combined exposures to surrounding green, air pollution and traffic noise on mental health. Environ Int. 2019;129:525-537. doi:10.1016/j.envint.2019.05.040
- Roberts S, Arseneault L, Barratt B, et al. Exploration of NO2and PM5 air pollution and mental health problems using high-resolution data in London-based children from a UK longitudinal cohort study. Psychiatry Res. 2019;272:8-17. doi:10.1016/j.psychres.2018.12.050
- Newbury JB, Arseneault L, Beevers S, et al. Association of Air Pollution Exposure With Psychotic Experiences During Adolescence. JAMA Psychiatry. 2019;76(6):614-623. doi:10.1001/jamapsychiatry.2019.0056
- Daiber A, Lelieveld J, Steven S, et al. The “exposome” concept – how environmental risk factors influence cardiovascular health. Acta Biochim Pol. 2019;66(3):269-283. doi:10.18388/abp.2019_2853
- Cabrera LY. Pesticides. Camb Q Healthc Ethics. 2017;26(4):602-615. doi:10.1017/S0963180117000111
- Shriver AJ, Cabrera LY, Illes J. Environmental Neuroethics: Bridging Environmental Ethics and Mental Health. Am J Bioeth. 2017;17(9):26-27. doi:10.1080/15265161.2017.1353172
